A look at precision medicine in Colombia
Friday 2 February 2024

A look at precision medicine in Colombia. High-cost account and cancer as a protagonist
Elsa Jenny Díaz López, MSc, Officer in Biochemistry, Molecular Biology and Biomedicine. Product Specialist of the Genetics line.
The High Cost Account (CAC), created by Decree 2699 of 2007 in Colombia. It is a non-governmental organization of the General System of Social Security in Health that brings together the national EPS, both of the subsidized and the contributory regime, to address the treatment of high-cost diseases that each of these entities is responsible for. The CAC operates as a self-managed fund to contribute to equity in health care for the population that is classified as having a chronic disease or poor prognosis.
Between 2019 and 2020, the high cost account reported cancer how a high incidence in both pediatric population (0 years to 19 years) and adult population (older than 19 onwards). Among the most frequent cancers in our country are: Prostate, colorectal, stomach, breast, cervix, melanoma, lymphoid leukemia and lymphomas. (7)(8) Early diagnosis of the population makes a difference in the survival rate of both pediatric and adult patients. However, to date this early detection is affected by the non-specific symptoms that may occur as well as compliance with the medical algorithm in which a number of routine tests must be performed in order to determine whether specialized tests and pathology are required to definitively diagnose the patient. In some cases, this period of time may take some time due to the authorization processes carried out by the EPS in which the patient is immersed, which delays the diagnosis.
Given the sustained pandemic in the country since 2020, the CAC has not yet provided recent figures. However, it would be important to contemplate medical algorithms that promote the use of new generation technology that promote epidemiological studies to classify the population with some risk of genetic predisposition in order to provide timely and effective treatments that have the effect of reducing health care costs for this type of population at the national level.
Actuality of the diagnosis and treatment of cancer in Colombia.
The genomic analysis applied to human diagnosis requires a blood or tissue sample to study the genetic material of either deoxyribonucleic acid (DNA) or ribonucleic acid (RNA) (11). This has been done worldwide since 1986, when the Human Genome Project was initiated, since at that time there were many questions of molecular and cellular aspect and at the same time it was suspected that the progression of a rare and terminal disease such as cancer was largely due to erroneous interactions of a large number of genes and molecules that intervene in biological cascades such as the cell cycle, DNA repair and protein production (2).
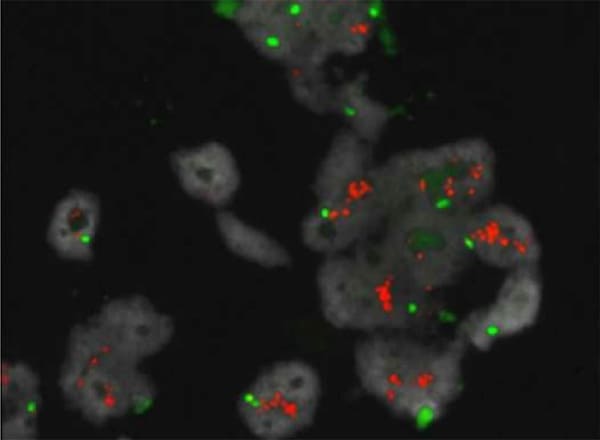
Image taken from https://metasystems-probes.com/en/probes/xl/d-6010-100-og/. Metasystems XL ERBB2 (HER2/NEU) amp probe hybridized to breast cancer tissue. Multiple orange signals indicate ERBB2 (HER2/NEU) amplification.
The above hypothesis was only resolved until 2003, when the complete sequence of the reference human genome was obtained, leading to a complete understanding of the nucleotide changes that lead to cancer progression(1). This was confirmed years later, between 2006 and 2008, when the “The Cancer Genome Atlas (TCGA) project, a landmark Cancer Genome program that molecularly characterized more than 20,000 primary cancer molecules and matched normal samples to elucidate cancer heterogeneity” (2) was initiated.
These data also have epidemiological relevance since they will also allow to characterize those families with a significant history of cancer, allowing the early recruitment of these patients, which indirectly reduces the cost of treatment at the EPS level.
The above example applies to several types of cancer that have a high incidence in the Colombian population among which are: Colon, stomach, prostate, melanoma, etc., but which, unlike breast cancer, are not yet described in the clinical practice guidelines for specific diagnostic and follow-up markers (6).
The cancer genome, therefore, is the specific alteration of a group of genes that may differ from patient to patient with the same type of cancer; today it is known that there are alterations that have to do with the activation or silencing of specific genes for each type of cancer, but that, at the same time within this molecular environment, it is particular to each patient since it may consist of a group of genes affected in the following cases
unique combination. Clinical oncology has relied on the increasing amount of molecular data that can be obtained from samples from individual patients with the condition (3).
Thus, the introduction of genetic panels at the oncology clinic level profiles genetic mutations for diagnostic purposes, selection of targeted therapies, treatment monitoring, prevention and classification of the population at risk (Familial Cancer Genetic History).
They are carried out using the second generation sequencing technique (Study of small fragments between 200 and 500 bp of the
DNA or RNA) and the third generation sequencing technique (study of fragments larger than 1000 bp of DNA or RNA) (4).

Genetic panels incorporate primers directed to specific targets that allow the study of the nucleotide order from 1 gene to 500 genes in the same individual at the same time, in order to identify changes in the DNA of pathological type (pathological variants) according to the classification of the American College of Medical Genetics and Genomics (ACMG, American College of Medical Genetics and Genomics), such as: Single Base Substitution (SBS), translocations, deletions, insertions and fusions, copy number change (CNV), Tumor Burden (TMB) however, to date this technique involves a high cost for EPS.
A strategic solution to target precision medicine in our Colombian population diagnosed with cancer of either tumor type (organ involvement) or hemato-oncology (blood cell alteration) is through the use of real-time PCR technique, this methodology represents a lower cost compared to the technique of second and third generation sequencing, allowing an initial approach to precision medicine.
Currently the PCR technique is standardized for use with kits that allow the identification of specific actionable genes such as BCR/ABL, JAK2, PIK3CA, FGFR, NRAS, BRAF and EGFR that are involved in therapeutic targets that account for personalized medicine for patients already diagnosed, leading in this way to a better survival for those patients who in the past were classified with a poor prognosis, but nowadays with the pharmacological advance, biological and immunological drugs have been generated that allow patients to be treated in a personalized way and according to the specific genomics of their cancer. (5)
In Colombia, the use of precision medicine is not yet well described in the protocols or medical practice guidelines. Likewise, it is limited to what is immersed in the CUPS, being this the guide in which the health system allows the use of innovation techniques in a timely manner. It is urgent that interdisciplinary groups in medicine (specialists) be formed in order to see the cancer patient as a unique being with multiple conditions that led to the pathological outcome he or she is experiencing.
A good example of the effective use of precision medicine in our country is when a woman diagnosed with breast cancer undergoes additional genomic tests to determine whether it is a Hormone Receptor (HR) positive and/or negative breast cancer, as well as the presence or absence of Human Epidermal Growth Factor 2 (HER2) in the tissue. (12) These data together with the age of onset of the disease will guide the way in which the treating physician decides on hormonal and/or biological therapy, the purpose of which is to slow the growth of the tumor prior to surgical intervention. In addition, in patients diagnosed with a family history of breast cancer or other types of breast cancer, a family history of breast cancer may also be considered.
The performance of a genetic test allows finding genomic targets of low and high penetrance, being relevant those of high penetrance since it refers to a probability between 50 to 90% of expressing the disease (phenotype) and transmitting it to their descendants, which will allow the clinician to decide what type of mastectomy is appropriate, if it is the one of both breasts or only the affected breast.(5) These data also have epidemiological relevance since they will also allow characterizing those families with a significant history of cancer, allowing the early recruitment of these patients, which directly reduces the cost of treatment at the EPS level.(7)
Read the complete article: A look at Precision Medicine in Colombia
Bibliographic references
1. https://genome.cshlp.org/content/23/7/1054.full
2. https://www.cancer.gov/about-nci/organization/ccg/research/structural-genomics/tcga
3. https://www.nature.com/articles/s41420-020-00373-0
4. https://www.elsevier.es/es-revista-diagnostico-prenatal-327-articulo-tecnologias-secuenciacion-nueva-generacion-diagnostico-
S2173412712000273
5. file:///C:/Users/diaz.elsa/Downloads/The_Genomic_Landscapes_of_Human_Breast_and_Colorec.pdf
6. https://www.mycancergenome.org/content/disease/breast-carcinoma/#
7. https://cuentadealtocosto.org/site/wp-content/uploads/2020/09/CANCER2019COM-3.pdf
8. book childhood cancer 2020.pdf
9. https://gco.iarc.fr/
10. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4863474/
11. https://revistanefrologia.com/es-metodos-diagnostico-genetico-enfermedades-renales-articulo-X2013757511002577
12. https://medicosgeneralescolombianos.com/images/Guias_2013/gpc_19prof_sal_camama.pdf



